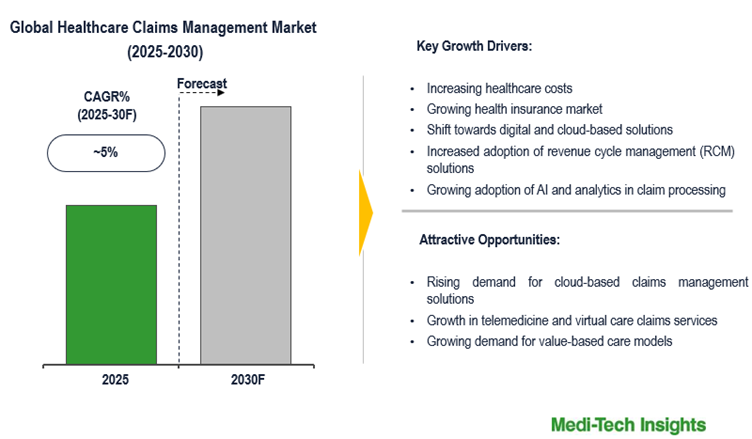
The healthcare claims management market is expected to expand at a CAGR of ~5% during the forecast period. Key growth drivers include increasing healthcare costs, a growing health insurance market, increased adoption of revenue cycle management (RCM) solutions, a shift towards digital and cloud-based solutions, growing adoption of AI and analytics in claim processing, a rise in value-based healthcare models, and the surge in telemedicine and remote healthcare services.
Healthcare claims management refers to the process of handling medical insurance claims, from initial submission to final reimbursement. It involves verifying patient information, coding medical procedures, ensuring compliance with regulations, processing payments, and managing denials or rejections. The goal is to streamline claim processing, reduce errors, prevent fraud, and ensure timely reimbursement for healthcare providers while maintaining compliance with insurance policies and government regulations.
🔗 Want deeper insights? Download the sample report here:
https://meditechinsights.com/healthcare-claims-management-market/request-sample/
Adoption of AI and analytics in healthcare insurance claims management drives market growth
Automation and AI technologies have become essential in healthcare insurance claims management, enabling insurers to streamline workflows, minimize manual tasks, and enhance accuracy. AI-powered chatbots and virtual assistants offer real-time customer support, while automated claims processing systems efficiently manage repetitive tasks like data entry and document handling. Additionally, AI-driven algorithms help detect fraudulent claims, allowing insurers to mitigate risks proactively. With vast amounts of data available, insurers are increasingly leveraging advanced analytics and predictive modeling to optimize claims management. By analyzing historical data, they can identify patterns, detect anomalies, and improve claim outcome predictions. Predictive modeling also enhances resource allocation, identifies high-risk claims, and accelerates settlements, leading to greater customer satisfaction and cost savings.
Adoption of AI and analytics in healthcare insurance claims management drives market growth
Automation and AI technologies have become essential in healthcare insurance claims management, enabling insurers to streamline workflows, minimize manual tasks, and enhance accuracy. AI-powered chatbots and virtual assistants offer real-time customer support, while automated claims processing systems efficiently manage repetitive tasks like data entry and document handling. Additionally, AI-driven algorithms help detect fraudulent claims, allowing insurers to mitigate risks proactively. With vast amounts of data available, insurers are increasingly leveraging advanced analytics and predictive modeling to optimize claims management. By analyzing historical data, they can identify patterns, detect anomalies, and improve claim outcome predictions. Predictive modeling also enhances resource allocation, identifies high-risk claims, and accelerates settlements, leading to greater customer satisfaction and cost savings.
Competitive Landscape Analysis
The global healthcare claims management market is marked by the presence of established and emerging market players such as McKesson Corporation; The SSI Group, Inc.; Quest Diagnostics; Kareo; Optum, Inc. (a subsidiary of UnitedHealth Group); Conifer Health Solutions; CareCloud; eClinicalWorks; IBM; Cerner Corporation; Oracle Corporation; Cognizant; and Change healthcare; among others. Some of the key strategies adopted by market players include new product development, strategic partnerships and collaborations, and investments.
Get PDF Report for Competitive Analysis:
https://meditechinsights.com/healthcare-claims-management-market/request-sample/
Market Segmentation
This report by Medi-Tech Insights provides the size of the global healthcare claims management market at the regional- and country-level from 2023 to 2030. The report further segments the market based on product, component, solution type, deployment mode, and end user.
- Market Size & Forecast (2023-2030), By Product, USD Million
- Medical Billing
- Professional Billing
- Institutional Billing
- Claims Processing
- Market Size & Forecast (2023-2030), By Component, USD Million
- Software
- Services
- Market Size & Forecast (2023-2030), By Solution Type, USD Million
-
- Integrated Solutions
- Standalone Solutions
- Market Size & Forecast (2023-2030), By Deployment Mode, USD Million
- On-Premise
- Web-Based
- Cloud-Based
- Market Size & Forecast (2023-2030), By End User, USD Million
-
- Healthcare Providers
- Healthcare Payers
- Others
- Market Size & Forecast (2023-2030), By Region, USD Million
- North America
- US
- Canada
- Europe
- UK
- Germany
- France
- Italy
- Spain
- Rest of Europe
- Asia Pacific
- China
- India
- Japan
- Rest of Asia Pacific
- Latin America
- Middle East & Africa
- North America
About Medi-Tech Insights
Medi-Tech Insights is a healthcare-focused business research & insights firm. Our clients include Fortune 500 companies, blue-chip investors & hyper-growth start-ups. We have completed 100+ projects in Digital Health, Healthcare IT, Medical Technology, Medical Devices & Pharma Services in the areas of market assessments, due diligence, competitive intelligence, market sizing and forecasting, pricing analysis & go-to-market strategy. Our methodology includes rigorous secondary research combined with deep-dive interviews with industry-leading CXO, VPs, and key demand/supply side decision-makers.
Contact:
Ruta Halde
Associate, Medi-Tech Insights
+32 498 86 80 79
info@meditechinsights.com